Metabolic-Genomic interactions in personalized medicine and therapeutic innovation of chronic inflammatory bowel diseases
Nutrition and microbiota as environmental triggers, metabolism, epigenome and innate immunity as modulators of cell reactivity and inflammation and cellular stress as damaging mechanisms are all part of the scenario behind outcomes related to inflammatory bowel diseases (IBD).
We will study the Nutrition- metabolism-epigenome-cellular stress interplay behind outcomes of IBD in animal models and cohorts. The final aim is to improve the quality of care of IBD patients thanks to the identification of new predictors and therapeutic innovation through a network of partnerships in the FHU ARRIMAGE.
The project is framed in 2 tasks: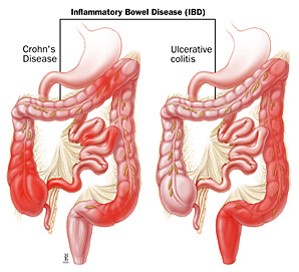
Epigenome-cellular stress-Innate immunity interplay behind outcomes of IBD: This task will decipher the cellular stress and RNA metabolism in our IBD experimental model of MDD rat subjected to DSS. We will study the expression and sub cellular mislocalization of HuR, with consequences on nucleo-cytoplasmic shuttles of RNA and adaptation to ER stress through the influence on SIRT1 expression. We will study the complementary role of RNA: pseudouridine-synthase hPUS10 and explore the interacting roles of ERAP1 and SIRT1 as modulators of ER stress in IBD. We will investigate the mechanisms contributing to pathological inflammation within the gut-joint axis, including gut microbiome (bacteria, viruses and fungi), using a multimodal approach from mice to humans and thanks to a regional collaborative effort in the Grand Est region.
Biomarkers in stratified medicine of IBD: We will identify new predictors of disease complications and efficacy and safety of biologics via an in-depth analysis of markers combined with omics approach to develop personalized therapeutics. We will use our regional (Nancy IBD cohort and TARGET project) and existing national (GETAID etc.) and European (ICARE etc.) prospective and well-characterized IBD cohorts with biobanking. The task will consider biomarkers identified from integrated analyses of omic studies of the methylome and the transcriptome in PBMC from IBD patients.
In collaboration with a private partner, Enterome, we will identify new markers having the ability to predict mucosal healing. All serum, genetic and fecal markers identified with the highest predictive value will be evaluated as candidates for inclusion in the MUCOSA index project.
Selected publications:
- Peyrin-Biroulet L, Gonzalez F, Dubuquoy L, Rousseaux C, Dubuquoy C, Decourcelle C, Saudemonmt A, tachon M, Béclin E, Odou MF, Neut C, Colombel JF, Desreumaux P. Mesenteric fat as source of C reactive protein and as a target for bacterial translocation in Crohn’s disease. Gut, 2012, 61, 78-85 (14.9)
- Peyrin-Biroulet L, Fiorino G, Buisson A, Danese S. First-line therapy in adult Crohn’s disease: who should receive anti-TNF agents? Nat. Rev. Gastroenterol. Hepatol., 2013, 10, 345-351 (IF 14.3)
- Bressenot A, Salleron J, Bastien C, Danese S, Boulagnon-Rombi C, Peyrin-Biroulet L. Comparing histological activity indexes in UC. Gut, 2015, 64, 1412-1418 (14.9)
- Lopez A, Cacoub P, Macdougall IC, Peyrin-Biroulet L Iron deficiency anaemia. Lancet, 2015, Aug 24. pii: S0140-6736(15)60865-0 (IF 44)
- Marchal-Bressenot A, Salleron J, Boulagnon-Rombi C, Bastien C, Cahn V, Cadiot G, Diebold MD, Danese S, Reinisch W, Schreiber S, Travis S, Peyrin-Biroulet L. Development and validation of the Nancy histological index for UC. Gut, 2015, Oct 13. pii: gutjnl-2015-310187. doi: 10.1136/gutjnl-2015-310187. (IF 14.9)